You’ve read the headlines. You’ve followed the studies. Your mind, sharp and endlessly curious, is always turning over the latest developments in science and medicine, especially when they intersect with the profound human struggle of addiction. Maybe it’s a personal battle. Maybe it’s someone you love. Or maybe, like so many of us drawn to this field, you’re simply captivated by the intricate, heartbreaking, and hopeful puzzle of the human brain under siege.
You know the old models. The 28-day rehab. The twelve steps. The white-knuckle fight of willpower against craving. You respect them, but you also know their limitations. You’ve felt the frustration of seeing a brilliant mind, a beautiful spirit, relentlessly hijacked by a primal need that logic and love seem powerless to touch. You’ve wondered, in your quieter moments, if there wasn’t something more, something that could quiet the screaming in the nervous system just long enough for therapy to actually take root.
What if the next frontier in addiction treatment isn’t a new form of talk therapy or a stricter rehab model, but a humble injection originally designed for type 2 diabetes?
Welcome to the surprising, burgeoning world of GLP-1 agonists—drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound)—and their potential to rewrite the story of substance use disorder. This isn’t just another medical headline; it’s a paradigm shift that speaks directly to your intellect and your hope for a more nuanced solution.
Beyond Willpower: Rewiring the Reward Circuitry
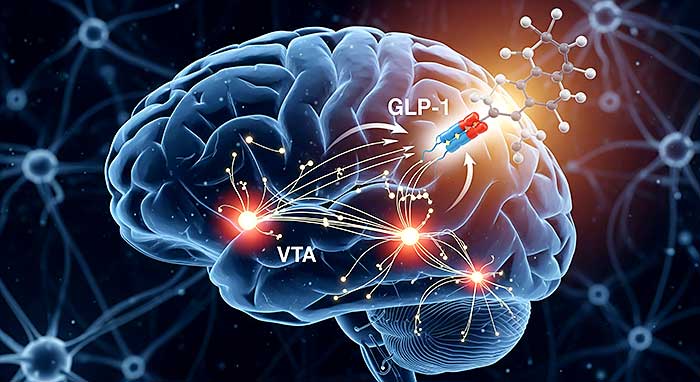
First, let’s talk science, because that’s where your mind lives. You understand that addiction is not a moral failing; it’s a chronic brain disease. It commandeers the mesolimbic pathway—the brain’s reward system. Dopamine, the neurotransmitter of pleasure and reinforcement, is flooded by substances like alcohol, opioids, or cocaine. The brain, in its amazing adaptability, downregulates its own dopamine production and receptors to compensate. The result? The addicted brain becomes incapable of feeling pleasure from natural rewards—food, sex, social connection—while simultaneously being bombarded with an all-consuming drive to seek the drug just to feel normal. The “why” behind the behavior is psychological, but the “can’t stop” is deeply, physically biological.
This is where GLP-1 drugs enter the picture. Their primary job is to mimic a gut hormone that regulates blood sugar and insulin. But the gut and the brain are in constant conversation via the vagus nerve. Researchers discovered that these drugs don’t just work in the pancreas; they cross the blood-brain barrier.
And what do they do there? They seem to turn down the volume on the dopamine signal itself.
Think of a craving as a deafening alarm bell clanging in your skull, drowning out every other thought. Traditional treatments might try to give you earplugs (willpower) or teach you meditation to ignore the sound (therapy). A GLP-1 agonist, however, appears to walk over and simply unplug the bell. It doesn’t just suppress appetite for food; it seems to blunt the obsessive, compulsive wanting that is the engine of addiction. Early preclinical studies on rodents, and now nascent human trials, are showing startling results: reductions in alcohol consumption, cocaine seeking, and opioid use.
The drug isn’t making you feel sick or averse to the substance, as with disulfiram (Antabuse). It’s not replacing the opioid, as with methadone or buprenorphine. It’s simply… quieting the noise. It’s creating space. For the first time in a long time, the mental chatter of “I need a drink” or “I have to use” begins to fade into the background.
The Space to Breathe, The Room to Heal
This is the part that will resonate with you on a deeply emotional level. You know that recovery isn’t just about stopping the substance; it’s about building a new life worth staying sober for. But how can you possibly do the hard, introspective work of therapy—processing trauma, building coping skills, mending relationships—when your brain is screaming at you 24/7?
The promise of GLP-1s is that they could provide the neurological peace necessary to actually do the work.
Imagine it. You wake up, and the first thought isn’t about your drug of choice. You drive past the old liquor store or your dealer’s street, and your hands don’t sweat on the wheel. Your heart doesn’t race. The siren’s call is a distant whisper, easily dismissed. In that silence, something miraculous can happen. You can finally hear your own thoughts. You can engage in a therapy session without your entire being focused on just making it through the hour without using. You can actually practice the mindfulness techniques your counselor taught you. You can feel the genuine, subtle joy of a conversation with a friend, or the taste of a good meal, because your brain’s reward system is no longer numb to everything but the drug.
This is the synergy that has experts so excited. It’s not a magic cure. It’s a tool—a potentially powerful one—that removes the biological barrier to healing, allowing the psychological and emotional work to finally land. It’s for the person who has been through rehab multiple times, who knows what they need to do intellectually, but whose body has consistently betrayed that knowledge.
A Future of Cautious, Intelligent Optimism
Of course, your critical mind is already raising flags. You’re right to. This is emerging science. The large-scale, double-blind, placebo-controlled human trials for substance use disorders are still in their early phases. There are side effects to consider—nausea, gastrointestinal issues—that can be significant. The long-term effects for this specific application are unknown. And crucially, this is not a stand-alone solution. It would be integrated into a comprehensive treatment plan that includes behavioral therapy and social support.
But the theoretical framework is sound. The anecdotal reports from people taking these drugs for weight loss, who have also experienced a sudden disappearance of long-standing addictive behaviors—from alcohol to compulsive shopping—are too numerous to ignore. The brain science is compelling.
For you, the intellectually engaged person who thinks deeply about addiction, this isn’t just a news story. It’s a validation. It confirms the complexity of the disease you’ve always known was there. It aligns with a modern, compassionate, and scientific understanding of why people struggle. It moves us further away from blame and further toward genuine, neurological healing.
It represents a future where treatment is personalized, where we can use every tool in the toolbox—from the molecular to the metaphysical—to help a person reclaim their life. It’s a future where we stop asking, “Why don’t you just stop?” and start asking, “How can we help quiet the storm inside your mind so you can find your way back to yourself?”
The revolution in addiction treatment might not come with a loud bang, but with a quieting of the internal noise that has tormented millions. It’s a hopeful, intelligent, and profoundly human step forward. And it’s a conversation you, with your keen mind and compassionate heart, are perfectly suited to understand. Keep watching this space. The best, it seems, is yet to come.
Citation
https://www.news-medical.net/health/Are-GLP-1-Drugs-the-Future-of-Alcohol-Addiction-Treatment.aspx